Dementia Care: A Partnership

Responsive Care Partnering is a type of dementia care partnership where the care partner:
- Is person-centered
- Is responsive
- Recognizes the value of non-drug options
Dementia Care is a Partnership
Dementia caregiving isn't just about the caregiver ... there's a team, or a partnership: the care partner and the person living with dementia (PlwD). When the PlwD is recognized as a part of the team,
- They feel more empowered
- They have less frustration
- Their symptoms decrease, especially those called" behavior and psychological symptoms of dementia" (BPSD).
For this to be a true partnership, care partners must
- Include the PlwD in decisions whenever possible
- Focus on remaining skills instead of those that are fading
Being Person-Centered
Care partners also need to be person-centered. This video talks about "Alzheimer's" but it speaks for all people with dementia. The Dementia Alliance is a group dedicated to making the U.S. a better place for people to live fully with dementia.
Person-Centered Matters: Making Life Better for Someone Living with Dementia, from The Dementia Alliance.
Care partners who see this journey from their loved one's point of view, not just their own, have better relationships with their loved ones, who in turn are happier and more content, with fewer BPSD. Responsive Care Partnering (RCP) means:
- Taking likes, dislikes and needs into consideration
- Being aware of underlying feelings
- Being alert for triggers, infections, hidden injuries and other discomforting event
Use this form or something similar to set up a baseline of "Who I Am." It can be fun to do with a loved one and can provide information for others so that they can provide person-centered care too.
- Life Story Questionnaire (pdf)
Being Responsive
The "R" in RCP, refers to being responsive to the PlwD's non-verbal communication as well as what they say: It means:
- Expanding communication recognition skills to include non-verbals
- Recognizing acting-out behavior as "stress-related communication," a call for help, and the start of a two-way conversation.
To be able to do these things, the care partner has to:
- Let go of old expectations and accept change (The RCP doesn't have to like it, but they do have to accept it.)
- Accept the PlwD's reality and suspend the need to assert one's own.
Non-Drug Options
These are the tools a care partner uses first with BPSD. The best course may often be a combination of drugs and non-drug options, where the RCP works with the doctors and therapists to find and monitor the best and safest combination. Check them all out and check find the best ones for your and your team.
- Download and use This Life Story Questionnaire for More Person-Centered Dementia Care. (From the Crisis Prevention Institute. (2016))
Being an Improv Actor:
Using improv to improve life with Alzheimers, from TEDMED
Improvisational theater, or improv, is where the drama is improvised on the spot without a script. When a care partner views irrational behaviors and psychological symptoms of dementia (BPSD) as an improv scene instead of "real life," it removes the need exert one's own reality with explaining, defending or arguing. This in turn allows the PlwD to feel validated and supported. Improv and RCP guidelines are very similar:
- Always say "yes." Accept the scene as given. This isn't true in the real world, but you are "on stage." As long as you can do so safely, agree to suspend your reality and accept theirs wholeheartedly, as any good actor would.
- Say "Yes, and...." That is, add something and move the action on. Respond with interest--but don't ask questions, which make your partner work too hard. "Wow! That sounds like you had a good time." Then, add something personal, to show that you really are invested. If it is an angry statement or accusation, respond to the feelings and then add an apology. "Oh, dear, no one should have to experience that. I am so sorry."
- There are no mistakes. Improv actors are flexible. They laugh at their mistakes and move on. Regroup and try again.
Using Improv with Dementia expands the subject further.
- usingimprov.pdf
Also this video extols the virtue of improv for the general public. It's long...over 11 minutes, but worth watching:
In The Moment is a website sponsored by Karen Stobbe, an improv actor with a mother who has Alzheimer's. It includes a six-session course on how to use improv with dementia. For more information about her organization and workshops, use the links below:
Care Partner Care
Caring for Elderly Parents at Home and Taking Care of Yourself, From Comforting Home Care - Bethlehem
It is easy to forget that the care partner is the PlwD's most valuable resource. A happy, relaxed care partner is the best "non-drug therapy" there is. When a care partner neglects their own care, stress follows. PlwD will respond to their care partner's stress with increased BPSD. Care partner care is not optional...it is a requirement! This list of ideas is just a start:
- Many non-drug options help the care partner too.Consider them treatments for both of you.
- Know when it is time to ask for help. Not getting help soon enough was the top mistake named by caregivers in a Lewy Warriors poll.
- Take regular time away from caregiving and spend it on yourself.
- Have a social life. Use the phone and the internet, but be sure some of it is in person.
- Get the legal and financial stuff taken care of early. It will save a lot of stress later.
- Take care of your physical health, making and keeping doctors appointments and following directions.
- Having an interest, other than caregiving-a hobby, volunteer, etc.
- Attending a support group, even if it is online. This may be the single most important self-caring thing a care partner does.
A support group offers ... a forum for learning and sharing with others who are on the same journey. You can vent and they understand. You can laugh and make dark jokes and they will laugh with you. A good support group is one of the best stress relievers there is. From Managing Cognitive Issues in Parkinson's and Lewy Body Dementia, by Helen and James Whitworth.
Quotes from group members:
- "This support group is my lifeline. I'd be lost without it."
- "I thought I was all alone, that no one else had the feelings that I had."
- "I learn something every time I go and it feels good to share what I've learned with others too."
- Members share support ("I've been there too"), information ("This is how I did that") and venting with people who understand.
- Learn where to find LBD support groups here.
Use this Caregiver Self Assessment form, provided by AGIS.com, to assess how well you are taking care of yourself. Be sure to read the suggestions for coping with stress at the bottom of the form.
- Caregiver Self-Assessment
- Caregiver Support Groups: 10/1/11 Rollercoaster blog - Groups can be local or online
- Our books.

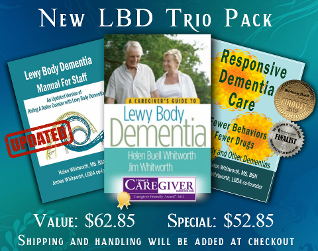
A Special Caregiver's LBDtools.com Offer!
This is a $62.85 Value for $52.85
THAT'S A $10.00 SAVINGS!
The Caregivers Guide to Lewy Body Dementia by award winning authors Helen and James Whitworth is the first book to present a thorough picture of Lewy body dementia in everyday language.
Responsive Dementia Care: Fewer Behaviors, Fewer Drugs provides family and professional caregivers with tools for dealing with difficult dementia-related behaviors.
This trio pack is rounded out with the UPDATED Riding a Rollercoaster With Lewy Body Dementia, the Whitworth's manual for caregivers of LBD patients.
Our Site:
Copyright 2014 - 2016: The Whitworths of Arizona - www.lbdtools.com - All Rights Reserved
site design by: